Alzheimer's Disease
Summary
- Progressive neurodegenerative disorder characterised by cognitive decline and memory loss
- Pathologically defined by accumulation of amyloid plaques and neurofibrillary tangles
- Imaging shows cortical atrophy, particularly in medial temporal lobes and hippocampi
Pathophysiology
- Accumulation of extracellular β-amyloid plaques
- Formation of intracellular neurofibrillary tangles composed of hyperphosphorylated tau protein
- Neuronal loss and synaptic dysfunction
- Neurotransmitter imbalances, particularly in cholinergic system
Demographics
- Most common cause of dementia, accounting for 60-80% of cases
- Prevalence increases with age:
- 3% in 65-74 year olds
- 17% in 75-84 year olds
- 32% in those 85 years and older
- Higher incidence in females
- Risk factors include:
- Advanced age
- Family history
- Apolipoprotein E ε4 allele
- Cardiovascular risk factors
- Lower educational attainment
Diagnosis
- Clinical assessment:
- Detailed history and cognitive evaluation
- Neurological examination
- Neuropsychological testing
- Exclusion of other causes of cognitive decline
- Biomarkers:
- Cerebral atrophy on imaging (see below)
- Cerebrospinal fluid (CSF) analysis for β-amyloid and tau proteins
- Genetic testing in familial cases
Imaging
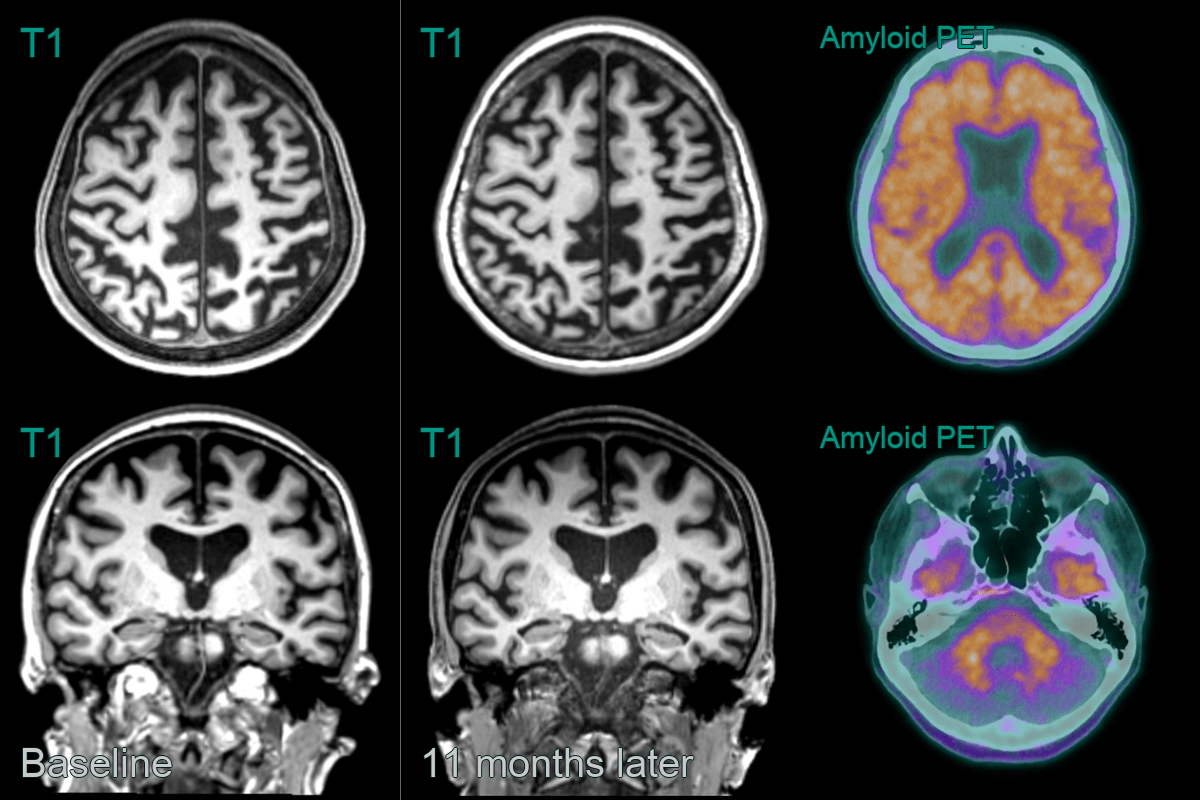
- 60-year-old patient presented with memory impairement. There was parietal and hippocampal (MTAS 2) volume loss. While the reduction in volume between the two scan was minimal, it was significant for such a short interval.
- Amyloid PET was postive with loss of supratentorial grey-white differentiation.
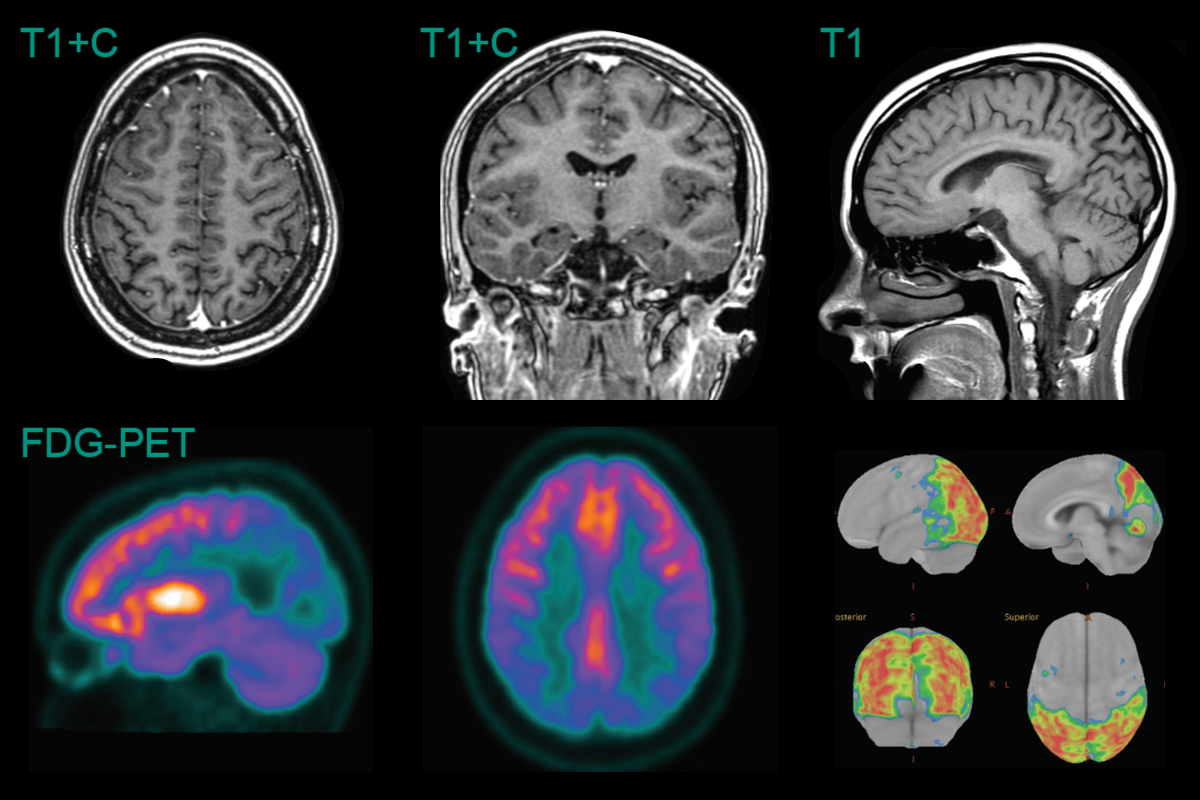
- A 30-year-old patient with a family history of Alzheimer's disease presented with cognitive impairment.
- While clearly abnormal for age, the volume loss in the parietal lobes was relatively mild. Hippocampal volume was within normal limits.
- FDG-PET showed marked hypometabolism in the parietal and occipital lobes. The Z-scores on standarised surface projection (Minoshima) maps were between -11 and -13.
Treatment
- Pharmacological:
- Acetylcholinesterase inhibitors (donepezil, rivastigmine, galantamine)
- NMDA receptor antagonist (memantine)
- Management of behavioural and psychological symptoms
- Supportive care and caregiver education
- Emerging therapies:
- Immunotherapies aimed at amyloid and tau clearance
Differential diagnosis
| Differential diagnosis | Differentiating feature |
|---|---|
| Vascular dementia | Stepwise decline, history of stroke or cardiovascular risk factors |
| Lewy body dementia | Visual hallucinations, parkinsonism, fluctuating cognition |
| Frontotemporal dementia | Early personality changes, language difficulties, younger age of onset |
| Normal pressure hydrocephalus | Gait disturbance, urinary incontinence, improvement with CSF drainage |
| Depression | Reversible cognitive impairment, mood symptoms predominate |
| Thyroid dysfunction | Abnormal thyroid function tests, reversible with treatment |