Cavernoma
Summary
- Cavernomas are vascular malformations composed of abnormal dilated blood vessels
- Typically found in the brain and spinal cord, they can cause seizures, haemorrhage, and neurological deficits
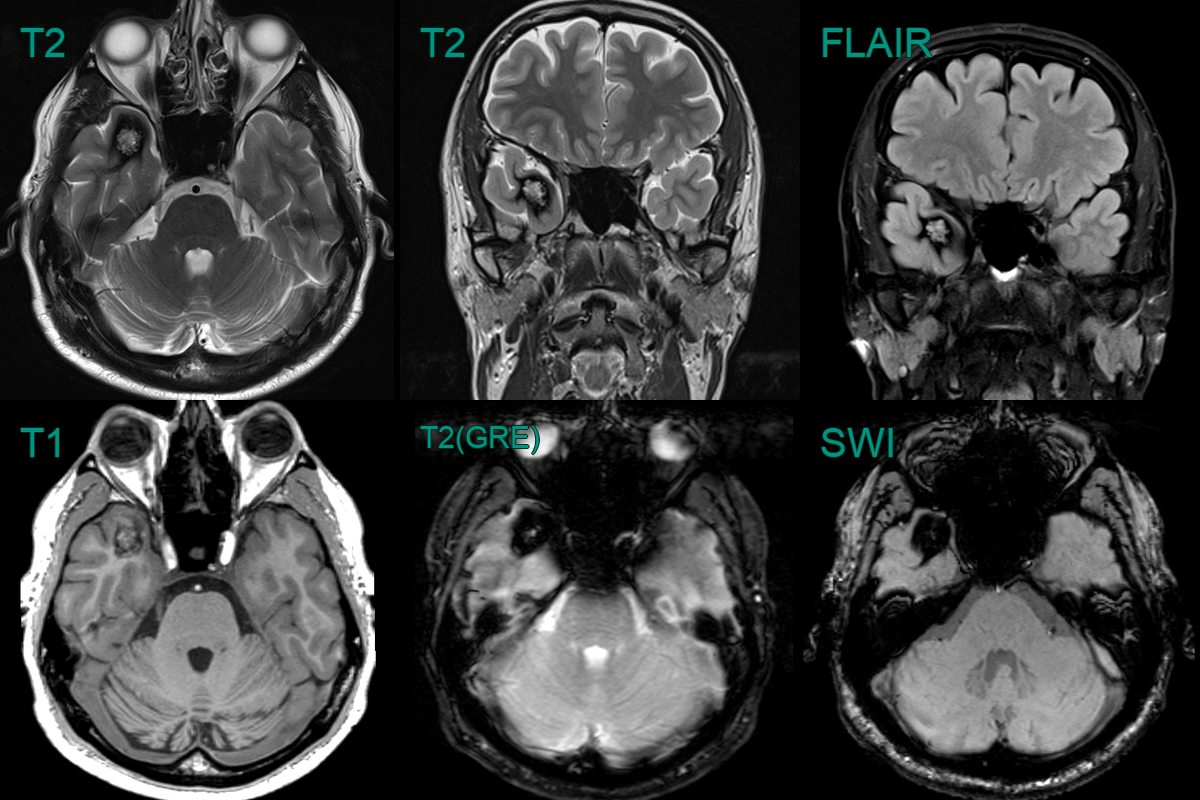
- Characteristically have a "popcorn" or "mulberry" appearance on T2-weighted imaging and hypointense on SWI
Pathophysiology
- Composed of closely packed, thin-walled capillary-like channels (caverns) lined by a single layer of endothelium
- Lack intervening brain parenchyma between vascular spaces
- Sporadic cases are more common, but familial forms exist (CCM1, CCM2, CCM3 genes)
- May be a delayed complication of radiation therapy
- Often asymptomatic but may cause seizures or neurological deficits after haemorrhage
Demographics
- Prevalence: 0.4-0.9% in the general population
- Can occur at any age, but most commonly diagnosed in young adults (20-40 years)
- No significant gender predilection
Diagnosis
- Often asymptomatic and discovered incidentally on imaging
- Can be difficult to identify if obscured by an acute haematoma
- Can occur alongside a developmental venous anomaly (~33% of cases)
Imaging
-
CT
- Potentially hyperdense due to calcification or acute haemorrhage
-
MRI
- T2 "Popcorn" or "mulberry" appearance with mixed signal intensity
- SWI Hypointense due to haemosiderin deposition and potentially calcification
- T1 Variable depending on presence or age of blood product
- ++T1+C++ Absent (or minimal) enhancement
-
Catheter angiogram
- Not visible on DSA ("angiographically occult")
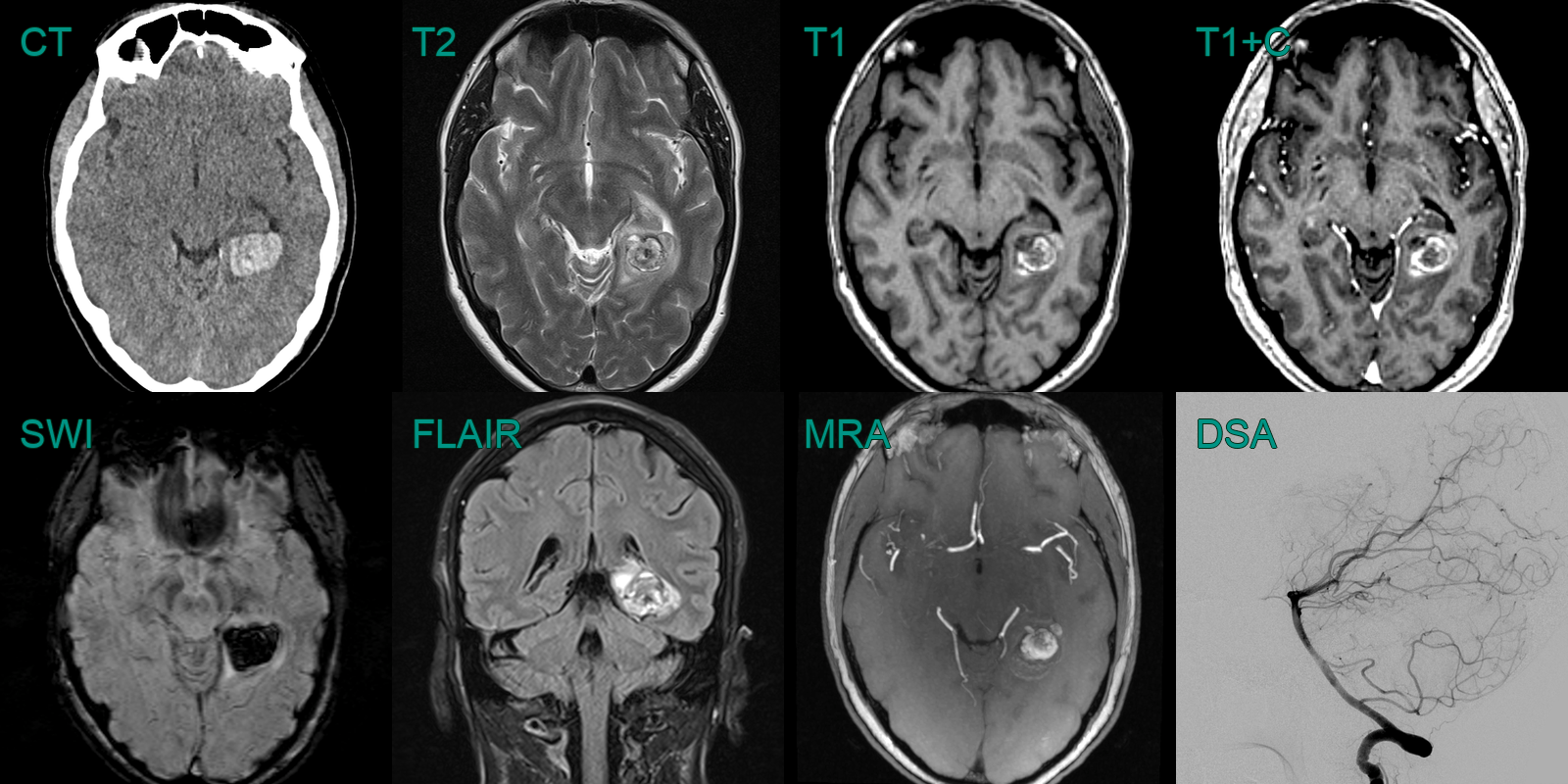
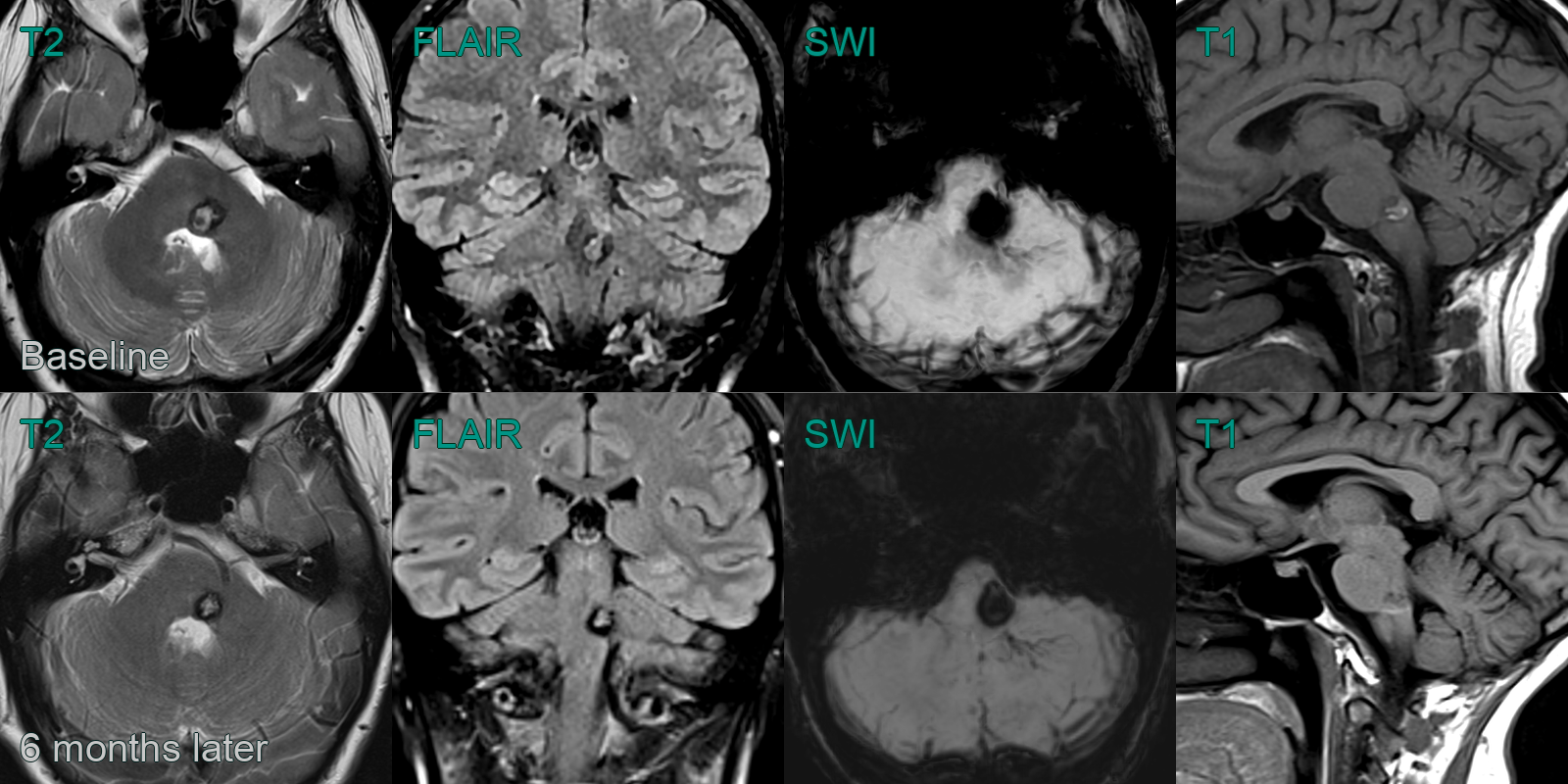
- A 30-year-old presented with left-sided facial weakness and numbness.
- The initial MRI showed a T1- and T2-hyperintense lesion in the left side of the pontine tegmentum, consistent with a recent haemorrhage within a cavernoma. SWI showed a network of small vessels representing an associated development venous anomaly
- 6 months later, mild rim of oedema on FLAIR, blooming artefact and T1-hyperintensity had regressed.
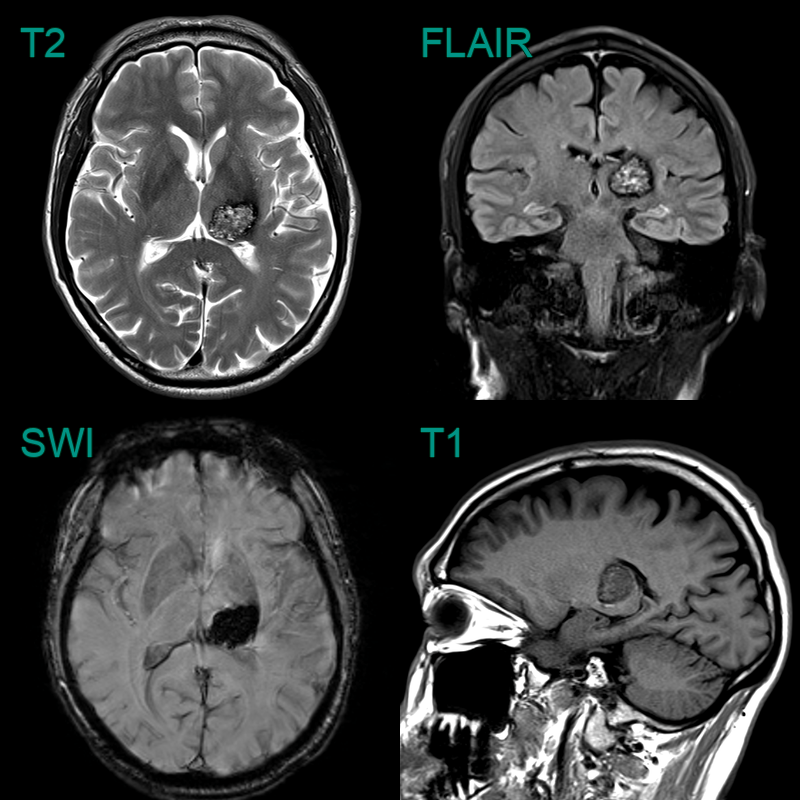
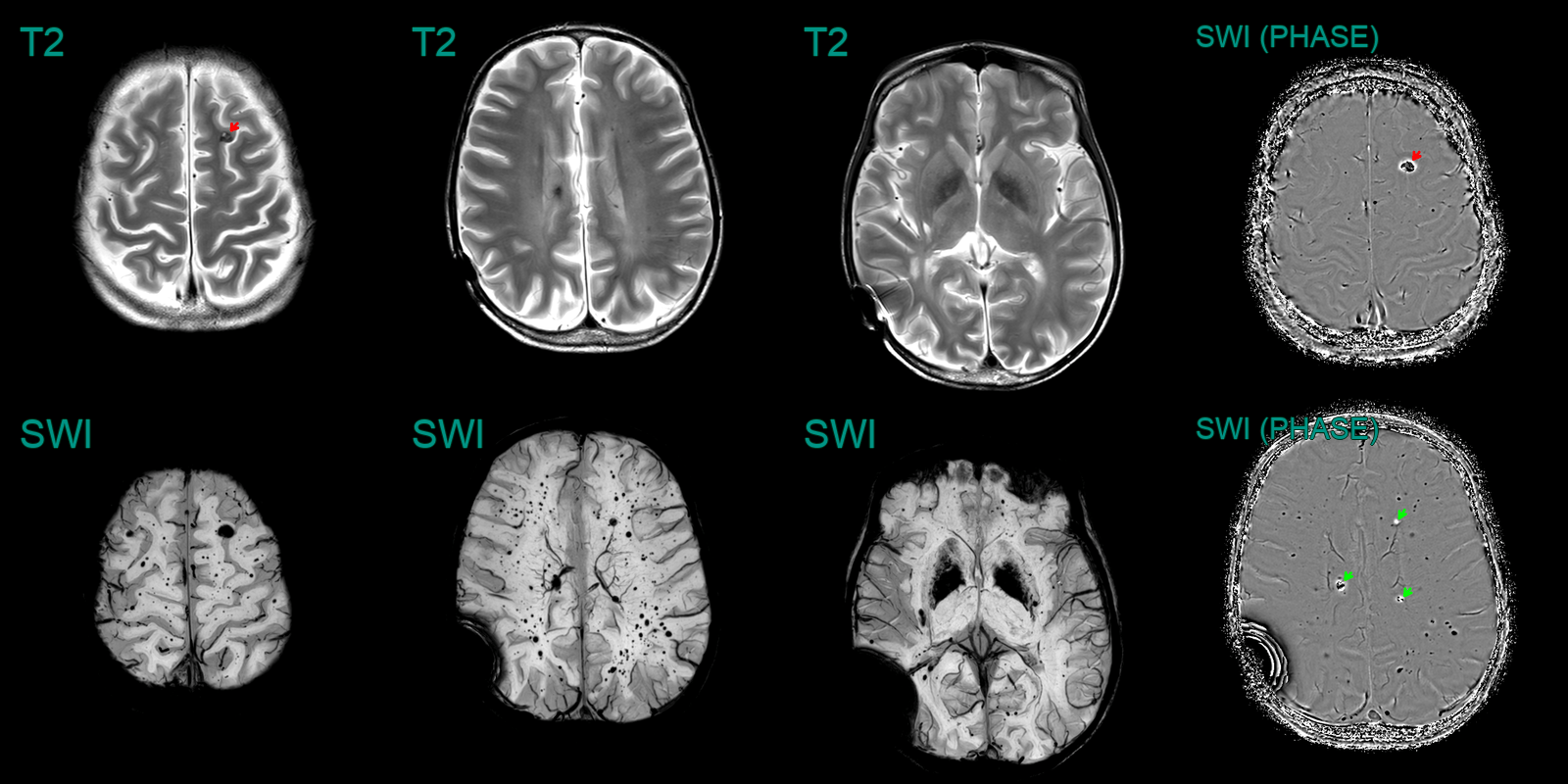
- A 25-year-old patient was treated with whole brain and spine radiotherapy due to a disseminated medulloblastoma.
- An MRI performed 10 years after treatment, showed extensive radiation induced changes including hazy white matter hyperintensity, multiple cavernomas (red arrow), microhaemorrhages and excessive mineralisation in the basal ganglia.
- The phase data from SWI showed mixed paramagnetic haemosiderin (black) and diamagnetic calcium (white).
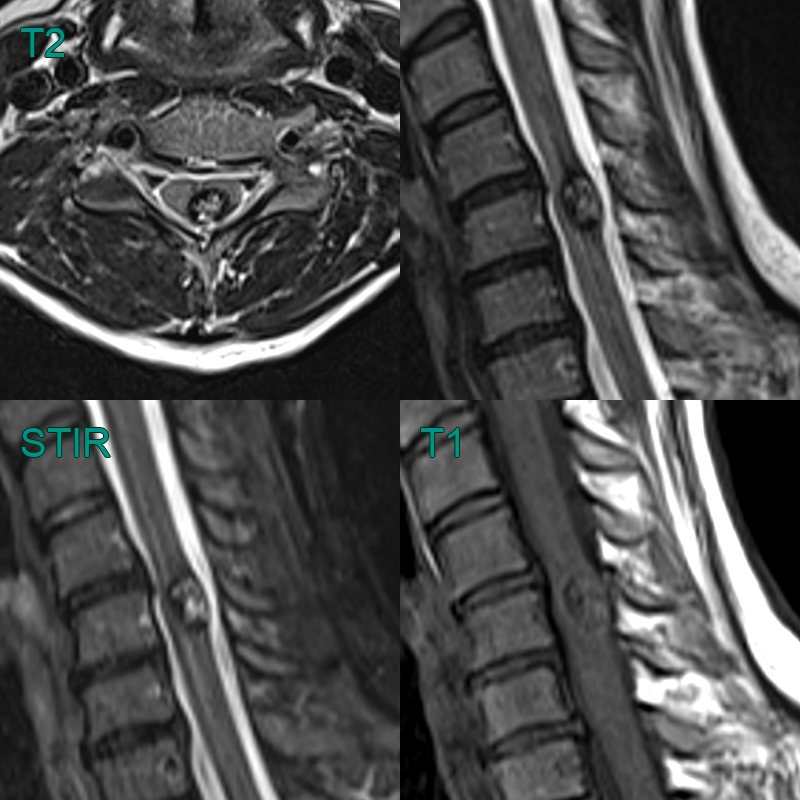
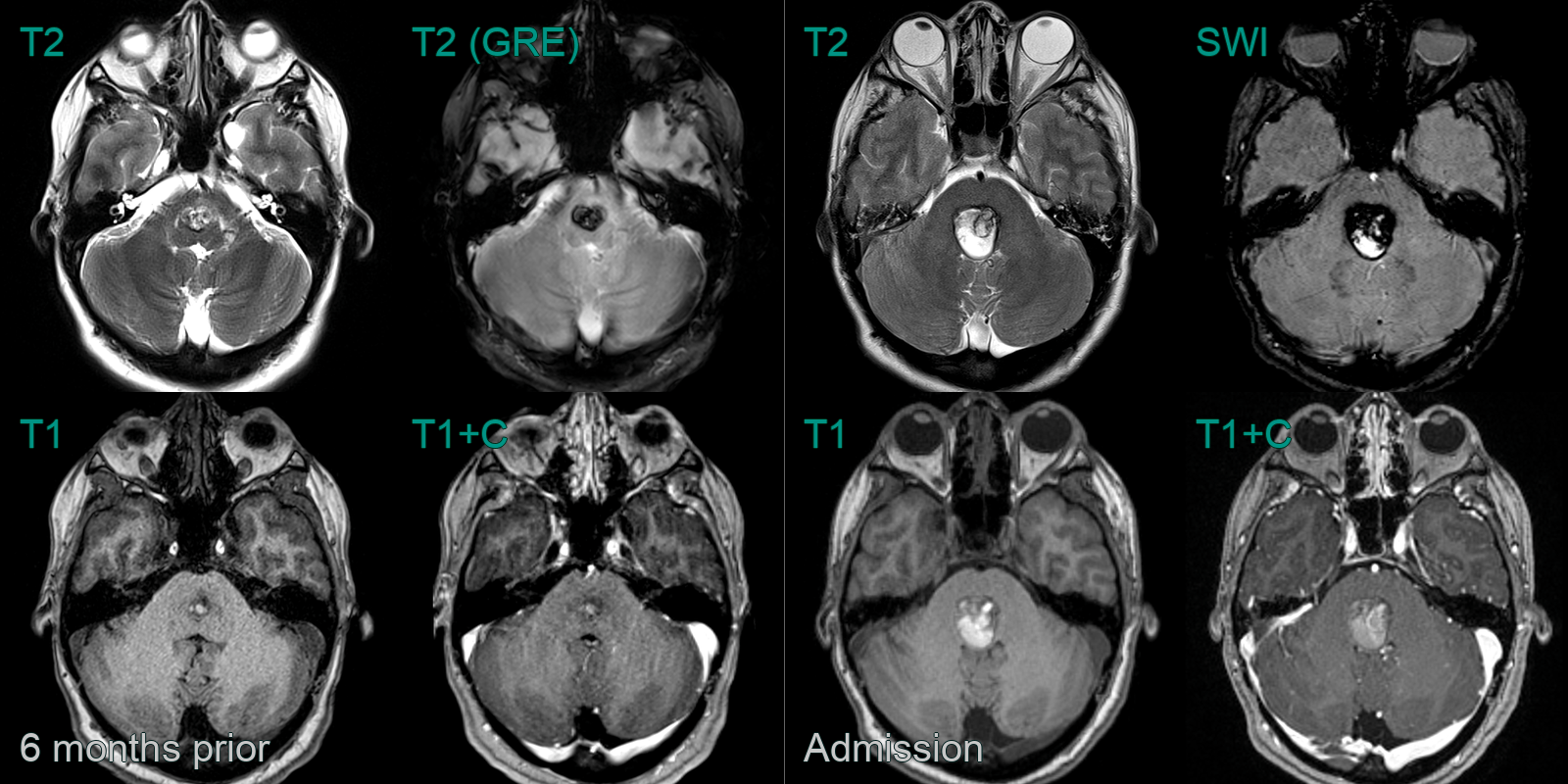
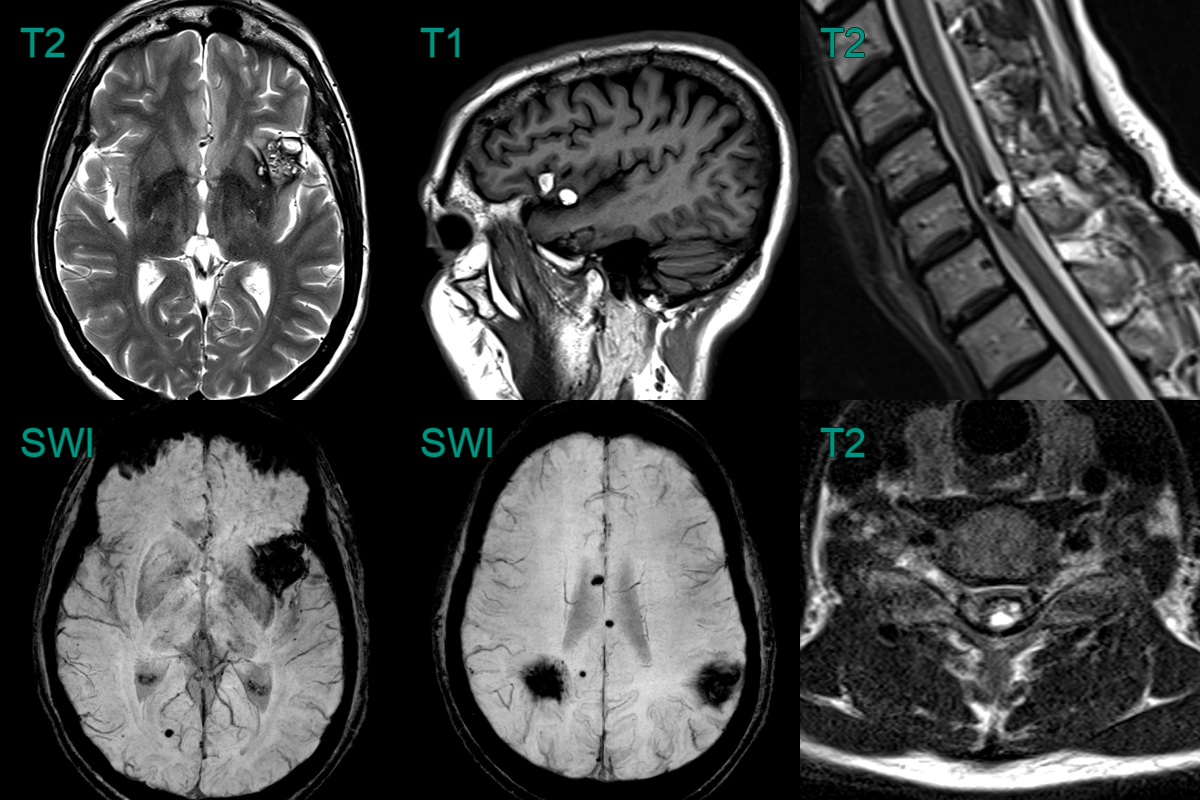
- A 40-year-old patient presented 2 years prior with headache.
- Initial imaging (not shown) showed a haematoma in the left insular region.
- MRI showed many other low intensity lesions within the brain and cervical cord representing cavernomas.
- The T1-shortening within the frontal operculum represented evolving blood product from the haemorrhage at presentation.
Treatment
- Observation:
- Asymptomatic lesions or those in eloquent brain areas
- Regular MRI follow-up to assess for haemorrhage or growth
- Surgical resection:
- Considered for symptomatic lesions (especially those causing seizures or repeated haemorrhage)
- Complete resection is curative
- Stereotactic radiosurgery:
- Alternative for deep-seated/surgically inaccessible lesions
- Can reduce haemorrhage risk but does not eliminate it
- Antiepileptic drugs:
- For seizure control in patients with epilepsy
- Genetic counseling:
- For familial cases to discuss inheritance patterns and screening of family members
Differential diagnosis
| Differential Diagnosis | Distinguishing Feature |
|---|---|
| Capillary telangiectasia | Typically smaller; lacks hemosiderin rim on MRI; classically in the pons; may show faint enhancement |
| Developmental venous anomaly | Can occur alongside a cavernoma; linear vascular flow void |
| Arteriovenous malformation | Flow voids on MRI; angiographic blush |
| Hemorrhagic metastasis | Multiple lesions; surrounding vasogenic oedema; identification of primary tumour |