Frontotemporal Dementia (FTD)
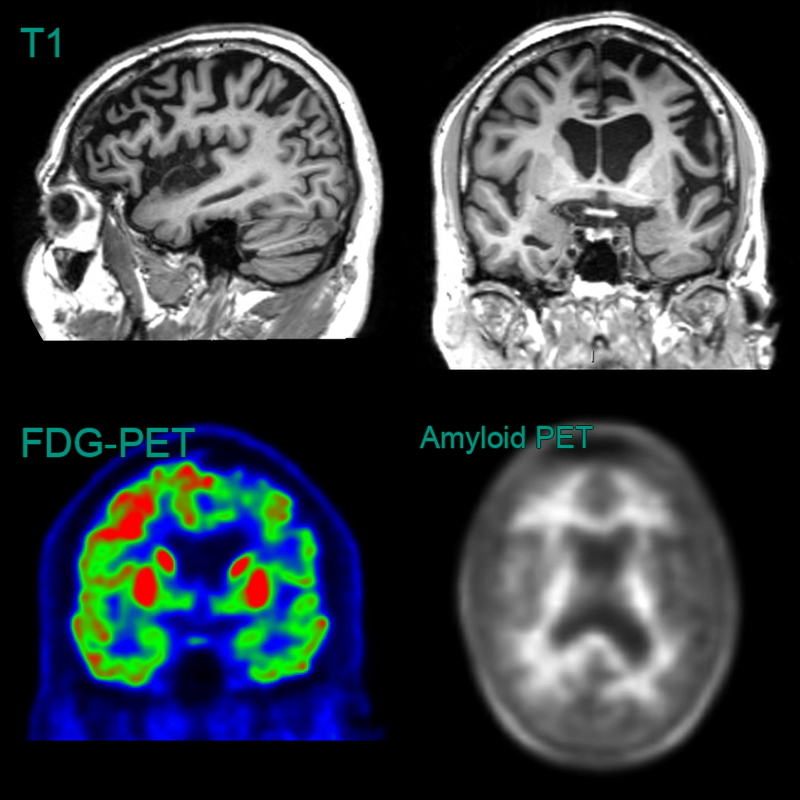
- 60-year-old patient presented with behavioural change and speech changes.
- MRI showed left frontal and temporal atrophy; the superior frontal gyrus was knife-blade thin.
- FDG-PET showed marked hypometabolism in the frontal and temporal lobes.
- Amyloid PET was negative with preserved grey-white matter differentiation.
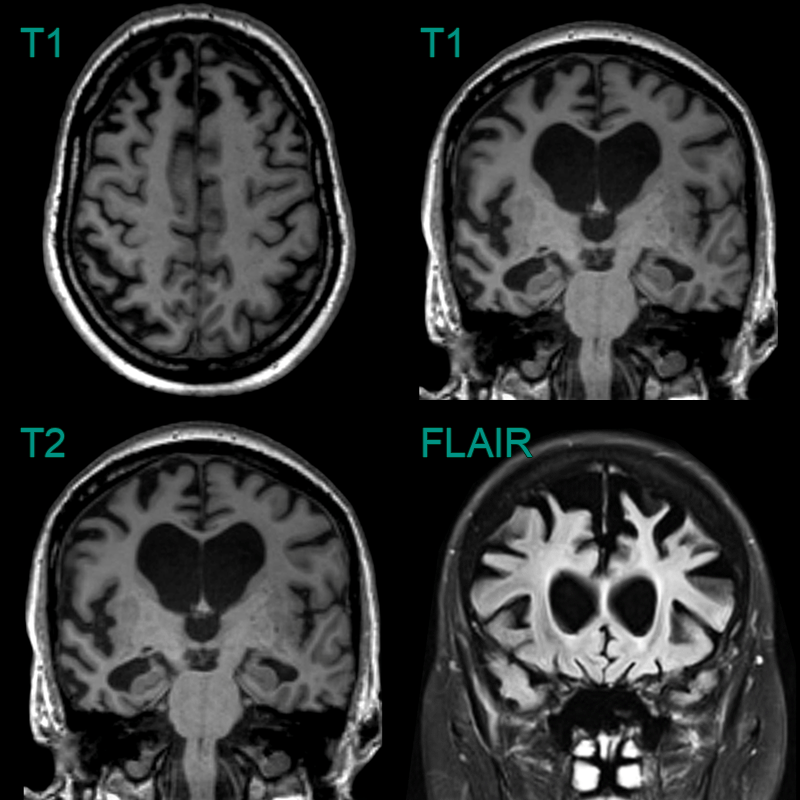
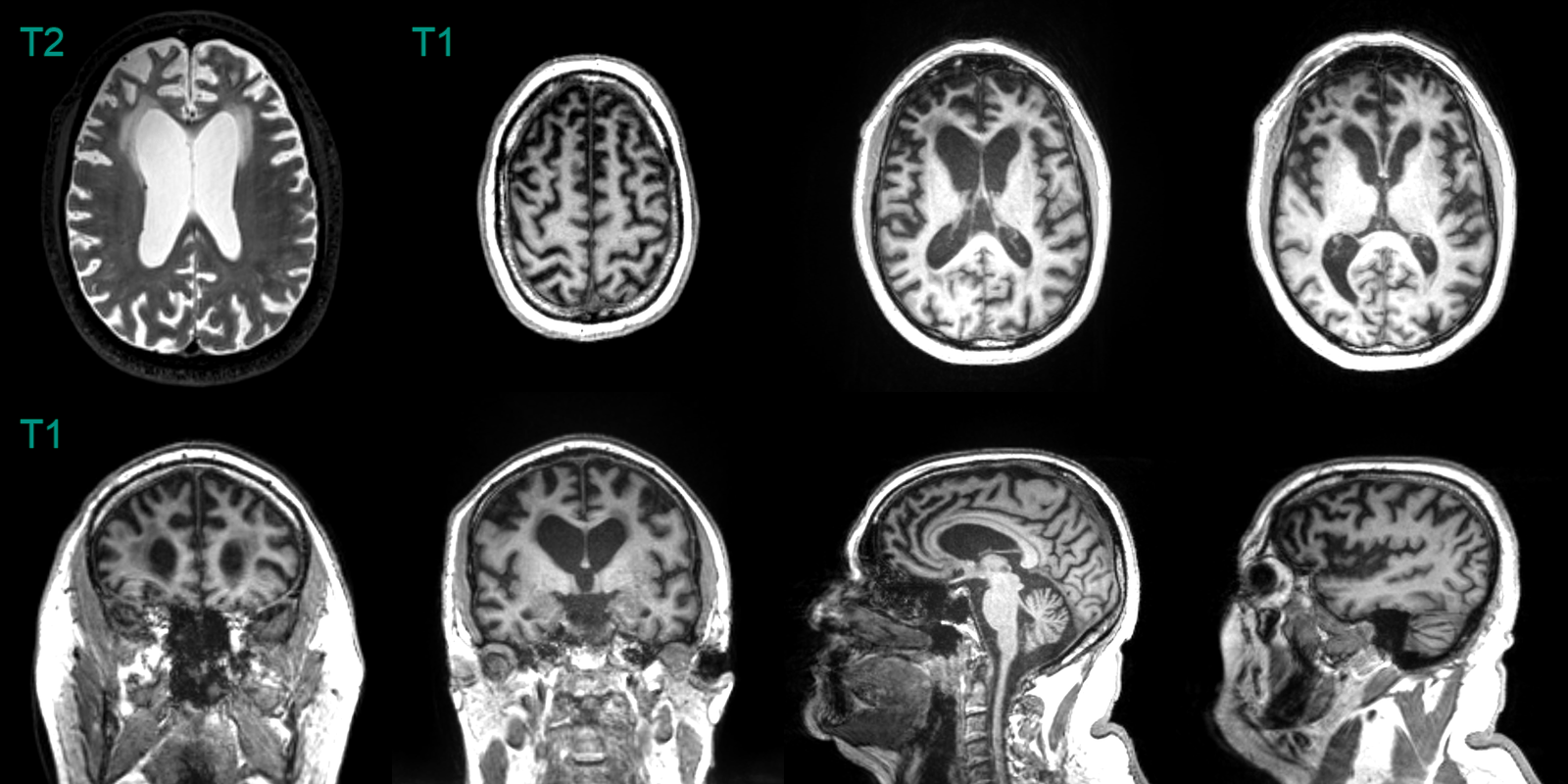
- A 60-year-old patient presented with disinhibition and impaired naming and verbal memory.
- MRI showed pronounced anterior temporal, milder left parietal, and no frontal lobe atrophy. There was particularly pronounced atrophy of the amygdalae.
- CSF amyloid markers were normal, making Alzheimer's disease unlikely. Genetic testing revealed a MAPT mutuation as the cause of frontotemporal dementia.
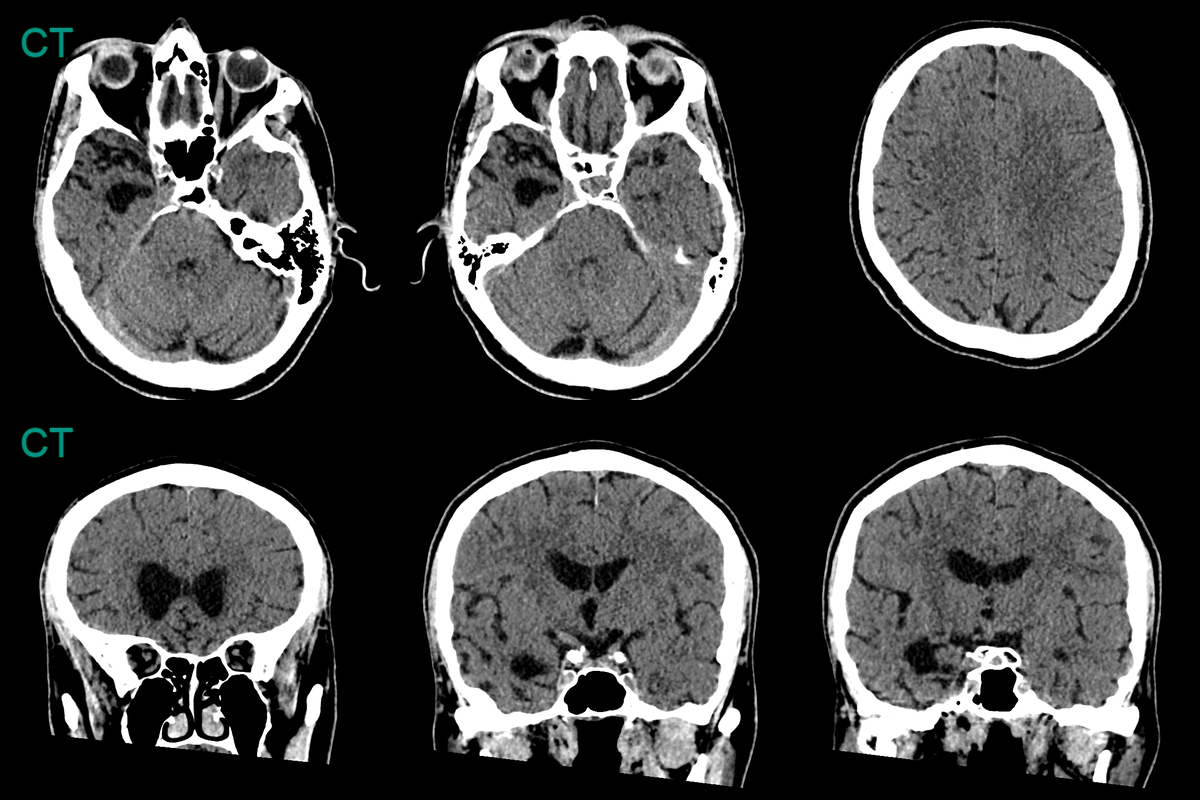
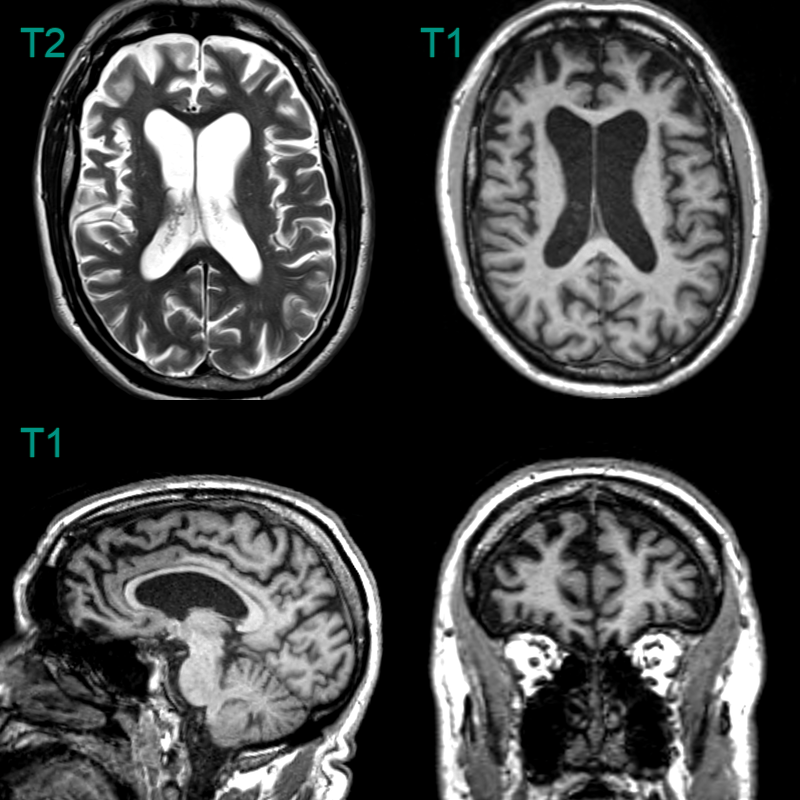
- A 60-year-old patient presented with apathy and increased weight. The patient's partner reported episodes of reckless spending in the preceeding year. The patient had a strong family history for dementia.
- MRI showed symmetrical frontal lobe atrophy. The frontal horns were larger than the trigones. The olfactory sulci were wided ("Crab sign").
- Genetic testing revealed a C9ORF72 mutation as the cause of the frontotemporal dementia.