Oligodendroglioma
Summary
- Oligodendroglioma is a slow-growing, diffusely infiltrating glial tumour of the central nervous system
- Typically affects adults in their 4th-5th decades of life
- Characterised by classic "fried egg" appearance histologically and 1p/19q co-deletion genetically
Cases
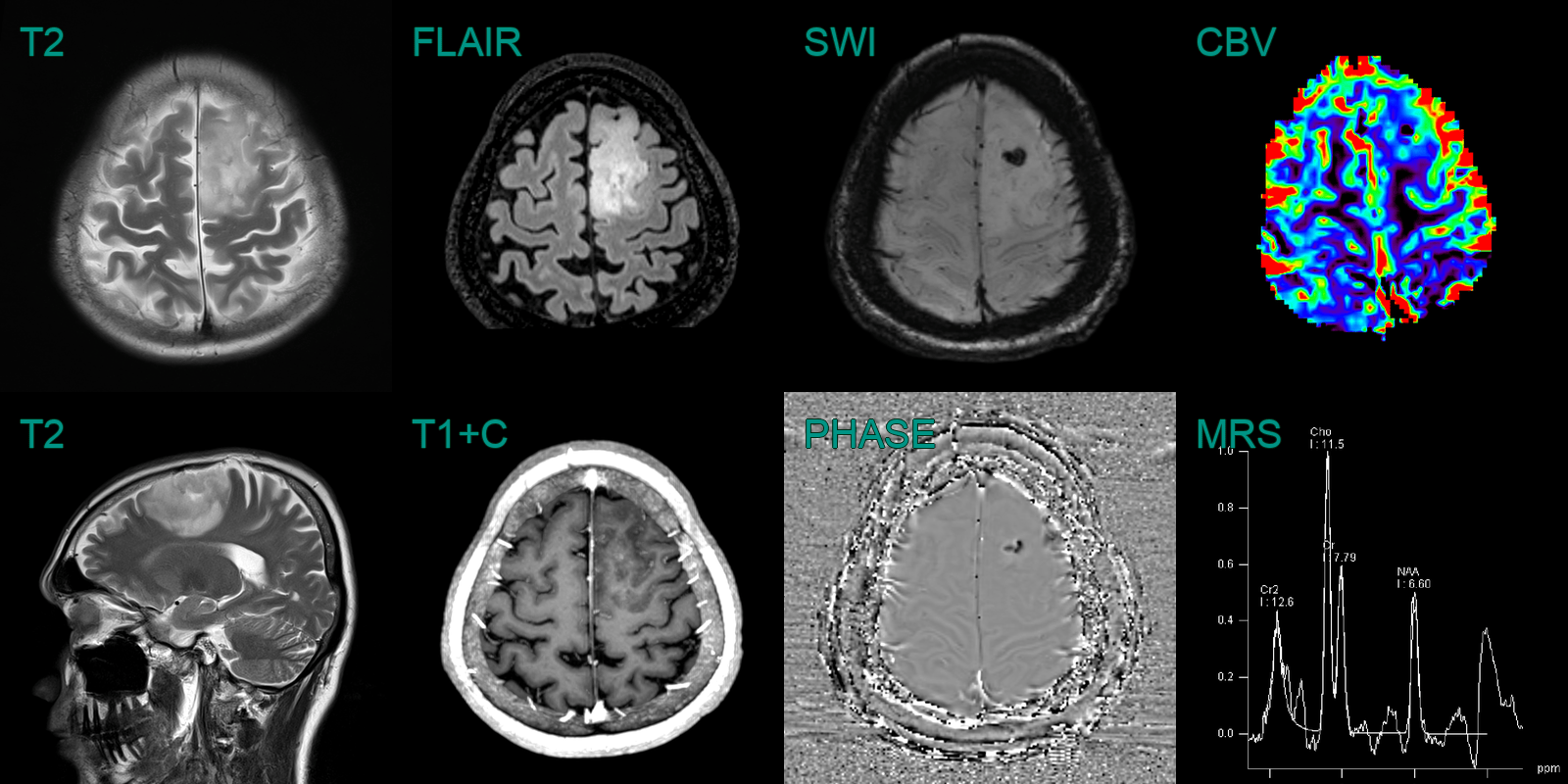
- A 40-year-old patient presented after a tonic-clonic seizure.
- MRI showed a relatively well-demarcated tumour in the left frontal lobe that involved cortex.
- Phase data from SWI showed diamagnetic susceptibility artefact consistent with dystrophic calcification.
- There was punctate enhancement and elevated CBV (ratio of 2.5 relative contralatera normal appearing brain tissue).
- MRS showed elevated choline and reduced NAA (indicating the replacement of normal neurons with mitotically active cells).
Pathophysiology
- Typically occurs in the cerebral hemispheres, particularly the frontal lobes
- Molecular markers include 1p and 19q co-deletion and IDH1/2 mutuation
- Typical findings of histopathological include "fried egg" oligodendrocytes, chicken-wire neovascularisation and microcalcification
Demographics
- Accounts for approximately 5-20% of all gliomas and 5-10% of all intracranial tumours
- Peak incidence in 4th-5th decades of life
- Slight male predominance (M:F ratio 1.1-2:1)
Diagnosis
- Clinical presentation:
- Seizures (50-80% of cases)
- Headaches
- Focal neurological deficits
- Cognitive changes
Imaging
- CT:
- Hypoattenuating cortical/subcortical mass
- Calcifications in 50-90% of cases
- May cause remodelling of the overlying skull (representing slow growth)
- MRI:
- ++T2/FLAIR++ hyperintense
- T1 hypointense to isointense
- T1+C Minimal to moderate enhancement with contrast
- SWI Hypointensity/blooming due to calcification (or, more rarely, haemorrhage)
- Advanced imaging:
- MR spectroscopy: elevated Cho/NAA ratio, presence of lactate/lipid peak
- Perfusion imaging: CBV may be elevated even in grade 2 lesions
Treatment
- Maximal safe surgical resection is the initial treatment of choice
- Adjuvant therapy based on grade and molecular profile:
- Grade II: observation or radiotherapy ± chemotherapy
- Grade III (anaplastic): radiotherapy + chemotherapy (typically PCV or temozolomide)
- Chemotherapy:
- PCV (procarbazine, lomustine, vincristine) regimen
- Temozolomide as an alternative
- Radiotherapy:
- Typically 54-60 Gy in 1.8-2 Gy fractions
- Prognosis:
- Generally better than astrocytomas
- 1p/19q co-deletion and IDH mutation associated with improved survival
- 5-year survival rates: 50-80% for grade II, 30-60% for grade III
Differential diagnosis
| Differential Diagnosis | Differentiating Feature |
|---|---|
| Astrocytoma | Lack of calcifications on imaging; less well demarcated/more infiltrative; absence of 1p/19q codeletion |
| Dysembryoplastic neuroepithelial tumor (DNET) | Cortical location; multinodular architecture |
| Ganglioglioma | Presence of neuronal component; lack of 1p/19q codeletion |
| Glioblastoma | Central necrosis and peripheral enhancement; lower ADC values reflecting hypercellularity |