Progressive Supranuclear Palsy (PSP)
Summary
- Progressive neurodegenerative disorder characterised by postural instability, supranuclear gaze palsy, and cognitive decline
- Pathologically defined by accumulation of tau protein in neurons and glial cells
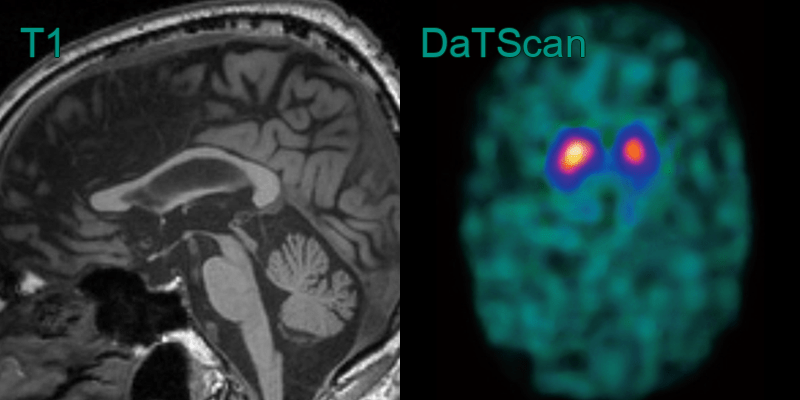
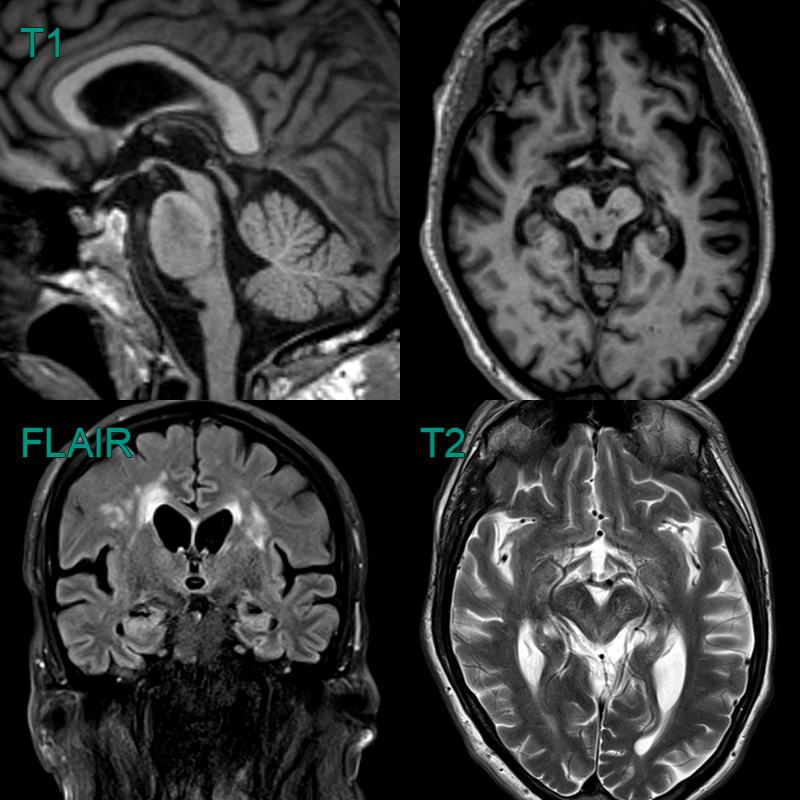
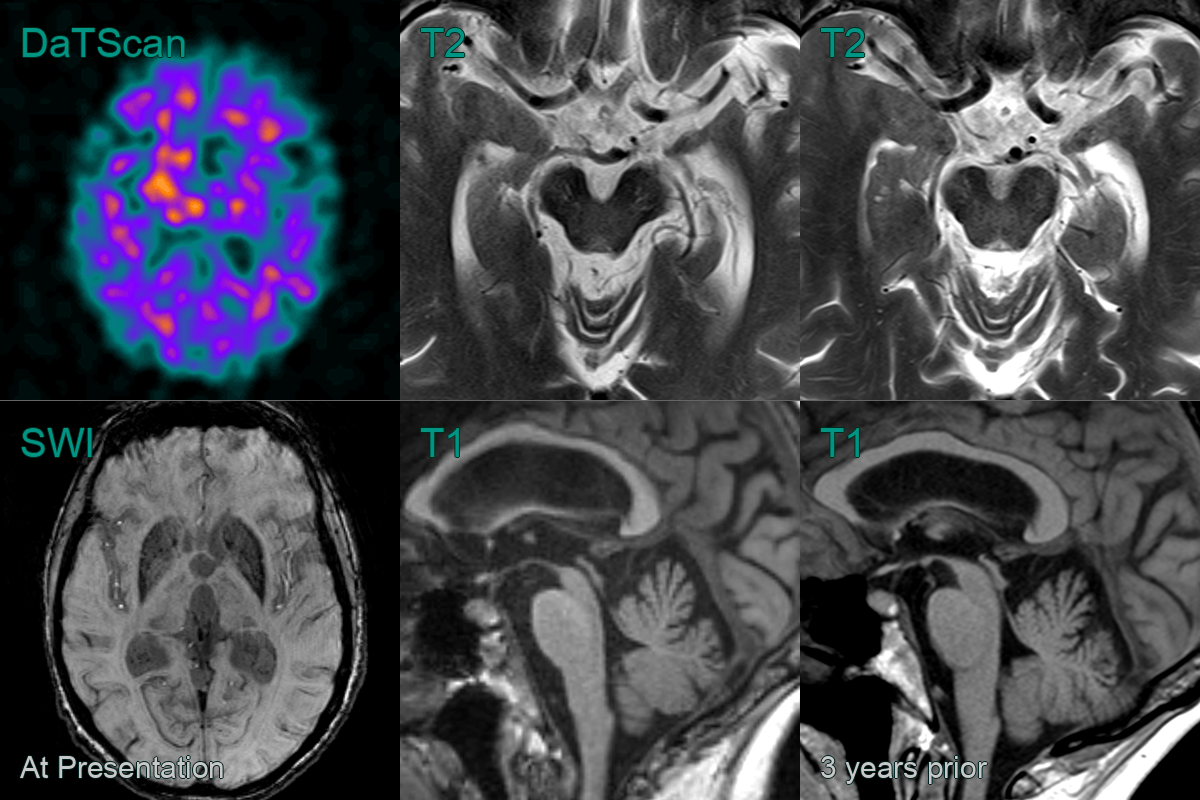
- Imaging shows midbrain atrophy with the 'hummingbird' sign in the sagittal plane
Pathophysiology
- Accumulation of hyperphosphorylated tau protein in neurons and glial cells
- Neuronal loss and gliosis in affected areas
- Familial cases associated with MAPT gene mutations
Demographics
- Typically affects individuals over 60 years of age
- Estimated prevalence of 5-6 per 100,000
- No clear ethnic or geographical predisposition
Diagnosis
- Clinical diagnosis based on:
- Progressive balance and gait disturbances
- Supranuclear gaze palsy, particularly affecting vertical eye movements
- Cognitive decline and behavioural changes
- Supportive features:
- Axial rigidity
- Dysphagia and dysarthria
- Frontal lobe signs
- Imaging shows excessive midbrain volume loss
- Definitive diagnosis requires neuropathological confirmation
Imaging
Treatment
- No curative treatment available
- Management focuses on symptomatic relief:
- Levodopa for parkinsonian symptoms (limited efficacy)
- Antidepressants for mood disorders
- Speech and language therapy for dysphagia and dysarthria
- Physiotherapy and occupational therapy for mobility and daily living activities
- Emerging experimental therapies:
- Tau-directed immunotherapies
- Microtubule stabilisers
Differential diagnosis
| Differential Diagnosis | Distinguishing Feature |
|---|---|
| Parkinson's Disease | Vertical gaze palsy in PSP; tremor more common in PD |
| Multiple System Atrophy | Cerebellar signs and autonomic dysfunction more prominent in MSA |
| Corticobasal Degeneration | Asymmetric limb apraxia and cortical sensory loss in CBD |
| Lewy Body Dementia | Visual hallucinations and fluctuating cognition more common in LBD |
| Normal Pressure Hydrocephalus | Urinary incontinence and magnetic gait in NPH |
| Vascular Parkinsonism | Stepwise progression and lower body involvement in vascular parkinsonism |
| Frontotemporal Dementia | Behavioral changes and language deficits more prominent in FTD |